Healthcare system overview | Health care system | Heatlh & Medicine | Dialogue between Salman Khan and Baker
Healthcare system overview | Health care system | Heatlh & Medicine
SALMAN KHAN: I'm here
with Professor Laurence Baker at Stanford
Medical School. And what we're going
to talk about now is the overview of the
health care system. LAURENCE BAKER: What is
the health care system? SALMAN KHAN: Yeah,
and who's in it? LAURENCE BAKER: And who's in it? And what are they doing? SALMAN KHAN: I think I
could give a go at it. LAURENCE BAKER: Go for it.
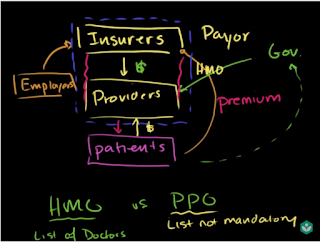
SALMAN KHAN: And
then correct me. Expose my ignorance. So clearly, you
have your providers. Those would be your doctors,
and nurses, and all the rest. LAURENCE BAKER:
Hospitals, pharmacies, all kinds of people
are your providers. SALMAN KHAN: OK, so everyone
who's providing health care.
So that's right over there. So that's hospitals, doctors,
pharmacies, all the rest. And then they are providing
the health care to someone. So those would be the patients. Let me do that in another color. LAURENCE BAKER:
Call them patients. Yeah, sometimes
you get the details
like people become patients
after they need health care. But some people just
have a question. They're not really patients,
they're just asking. SALMAN KHAN: OK. What would you call them then? LAURENCE BAKER: Call
them population. SALMAN KHAN: Population. So just the population of
the world, or of the country, or whatever-- people. And then someone
has to pay for this.
And so for the most
part, this is insurers. LAURENCE BAKER: Yup. Insurance companies. In the olden days--
like if you go back 100 years-- we didn't
really have insurers. We had patients and providers. And patients would-- if they had
a question, they had a concern, they go to the provider. They'd make some deal,
pay them some money,
do some service for
them and work it out. We got insurance
companies really only in the last
100 years, maybe. Really starting in
the US in maybe 1930. 1940, they started
to become popular. So that's kind of
a new renovation. And those three
things work together. SALMAN KHAN: And the
general term-- and this is a word I've seen a
lot, and sometimes it's
a little confusing because
it's very close to payer, you hear of these payors. And that would be
including anyone who's paying for the
paying for the service. And insurance companies
would be included there. LAURENCE BAKER: Right.
So we have-- we
call them payors. Sometimes we call
them health plans because they arrange for some
of the care that people get. And payors could be private
insurance companies, or they could be government
payors-- government insurance companies like Medicare. SALMAN KHAN: And the insurance
companies themselves,
they're not doing this out of
the goodness of their heart. Someone is paying them. And for the most part
in the United States, it tends to be employers. LAURENCE BAKER: So right. So if we made another
arrow on your diagram here, it would be from
the population-- or maybe from the patients--
to the insurance companies that
provides the money for
the insurance companies to use to pay for the provider. So patients might buy
an insurance company-- or not an insurance company,
buy an insurance policy. SALMAN KHAN: Only if
they're very well healed. LAURENCE BAKER: Some of
them buy the whole thing. But they just might
buy their own policy. Go buy an insurance policy,
pay them a premium directly,
the insurance company
collects that money. Or, for most people, they
work for an employer. The employer makes
the arrangement to buy that insurance and
then implicitly charges the population, the
patients for that. Maybe directly by
having them contribute some of their salary.
Maybe implicitly by just
reducing the amount of cash they give them every
month, and instead giving them this
insurance policy. So people do that. And the other piece that's
floating around in here is that in some cases,
the population pays taxes to the government that
then functions essentially
as an insurer, like the
Medicare program, where there's insurance provided to people
that's paid for by taxes. So there's some different
funds flows going around here, but always money
going from patients to insurers, through employers
from taxes, by direct payments. Those insurers
collecting the money and then paying for a
bunch of the care that's
provided by the providers. And that's the
basic arrangement. There's one more
tiny piece, which is that sometimes patients pay
the doctors or the hospitals directly. You go you have
a $20 co-payment. And so there's a small payment
that goes back and forth. SALMAN KHAN: Your
copay is kind of there just so that-- it kind of makes
the insurance company feel
good that you're not just
using it willy-nilly-- that you have to
pay your $10 or $50. LAURENCE BAKER: Absolutely. So insurers know
that once they start paying the providers
for the care, and the patient says
it's totally free, people might use
stuff that might be worth a little tiny bit, but
it costs a lot for everybody to pay for.
So if you put a
co-payment on there, it makes people think
twice about using things that they don't really need. SALMAN KHAN: Right. That makes complete sense. And then within this ecosystem--
we hear a lot about HMOs. My perception is that's a
combination of the insurance company and the provider. It's kind of in one package. LAURENCE BAKER: Right.
So over time, the US has had
different kinds of insurers out there. In the private market,
especially, there's been a lot of innovation
in the last 30, 40 years in types of
insurers that are out there. So we have different
insurers that have behaved in
different ways as we've
gone through those
evolutionary cycles. So one version of that is
what we call an HMO-- a health maintenance organization. And that's really just jargon. You have to dig into it to
figure out what it means. But in a lot of
cases, what that is is a company that's
acting as insurance.
So you pay a premium to them if
you're a patient or a person, and you buy some coverage. And then they'll
cover your care. But they'll do that by trying
to integrate themselves with the providers. And so the
organizations either are integrated because the HMO hires
doctors directly, or maybe owns
the hospitals-- like Kaiser
Permanente, for example. Or, in some cases it's a
contractual relationship. It's not exactly the same. SALMAN KHAN: So not all of them
is tightly linked as a Kaiser, where it's like, you go
to this building that says Kaiser on it. And that's where your doctor is. It could be doctors just
have their practices,
but they're tightly
linked with a-- I think that's how, what Blue Shield? Or one of those. LAURENCE BAKER: Yeah,
Blue Shield, or Aetna, or some of these
different companies. And you can start to
dig into the details and every one will be a little
bit different from the other, but they're contractual
relationships. SALMAN KHAN: And
the difference-- I think this is something
everyone faces when they sign
up with insurance
with their employer-- I had to do it recently--
is-- they all say, you have to pick HMO versus PPO. And they're within
the same policy. And so my perception is HMO is
you have set list of doctors
that they probably
pre-negotiated pricing with. LAURENCE BAKER: Yeah. So the difference
between HMOs and PPOs gets a little bit
into the details SALMAN KHAN: OK. I don't want to get too into-- LAURENCE BAKER: We can sort
of think about it in the way that you're talking about it. So an HMO will have
a list of doctors that you're supposed to see.
And you'll have to go see
the doctors on that list. And a stereotypical one, if
you don't see the doctors on that list, the
insurance company's not going to pay
for you care, you're going to pay for yourself. And in the stereotypical
HMO, there's going to be a fairly
tight management between the insurance company
and the doctors about what's
going to be done, what's
allowable, and so on. SALMAN KHAN: And in the
most tightly linked case, they'll be the same. They doctors will be
employed by the company. That's like Kaiser. LAURENCE BAKER: As you think
about it as a spectrum, if you move a little bit
away from that to a PPO. What's happening in
a PPO is you're still going to get a list,
so you're going to be encouraged to
see those doctors,
but maybe it'll be a
little more flexibility. Like, if you decided not
to see someone on the list, the plan would still
pay some amount. Maybe not as much as they would
if you saw someone on a list, but something. Whereas in an HMO,
maybe nothing. And the plan will probably
work a little less hard
at managing what those doctors
are doing to try and limit access to, say,
high cost services. HMO will tend to
work harder, PPO tends to work a
little less hard. So it's a little
bit of a spectrum. You're kind of moving from more
managed and more concentrated to a little less managed, but
still more so than the system
we had, say, in
the '50s or '60s, where anybody went
to any doctor, and any doctor did
whatever they wanted. And the insurance company
just paid the bill, and there was no integration. So it's a little bit of a-- SALMAN KHAN: So that's
the main motivation why insurance
companies are trying to get more integrated
with the providers,
is because-- just like you
said, in the '50s and '60s, you have the provider
providing a service. And obviously the
patient like the service. And then you have a third
party paying for it. And so there's no check
on-- the person deciding and the person getting it says,
yeah, let's get more service. And someone else is-- right.
LAURENCE BAKER: So we
created a big issue. Insurance companies are
kind of an interesting thing in a health policy world. Because we have to have them. We have to have them to
manage the risk associated with getting sick. You get sick today
and get a huge bill. And so we can't leave people
on their own for that. We got to have
insurance companies. But as soon as you create
insurance companies,
and I can have, implicitly,
all my neighbors pay for the health
care that I want, then I might start using things that
turn out to be an efficient. And so you got to have
them-- insurance companies. But you got to manage what
happens when you have them also. And so that's the
integration between providers